Addiction Medicine
The Department of Addiction Medicine at St Vincent's provides medical treatment for drug or alcohol addiction. Our work includes direct patient treatment, research, education/training and policy development.
Addiction Medicine at St Vincent’s strives to ensure that our clinical knowledge and experience informs public health policy, to achieve a more sophisticated understanding in the community of the nature and treatment of addiction, and to improve the health outcomes for those seeking assistance for drug or alcohol problems.
The science of addiction
Today
addiction is widely understood to be a chronic, relapsing neurobiological
disease.
Genetic
variables, environmental factors, stress, and conditioning effects all
contribute to the progression from substance use to addiction and are also
recognised to be major factors mediating response to treatment.
Progression
from use/abuse to addiction is accompanied by long-term neuroadaptations and
these underlie persistent cravings and withdrawal symptoms, increase the risk
of relapse, and contribute to the cyclical nature of addiction treatment.
Persons
presenting for substance abuse treatment commonly have comorbid mental health
problems, and other general health problems that need to be addressed.
Central
to the treatment of addiction are three domains:
- Pharmacotherapy
- Psychosocial stability
- Behavioural interventions
Our Services
The following clinical services are delivered or administered from 62 Gertrude Street, Fitzroy 3065.
- Outpatient Clinics - Medical (assessments, secondary consultations, shared care), Counselling
- Consultation/Liaison Service
- Relapse Prevention Groups (for existing and past patients)
- Peer Support services
- SMART Recovery groups
- Provision of treatment under the Severe Substance Dependence Treatment Act (SSDTA)
Depaul House is a 12 bed community residential medically supervised withdrawal unit attached to St Vincent’s. The unit is staffed 24hrs by registered nurses, enrolled nurses, welfare workers and peer workers. This provides specialist care for those who wish to voluntarily undertake withdrawal from substances in a safe, clinical environment. We offer medically supervised withdrawal supported by a therapeutic group program and community engagement.
Access to Depaul House is now through community assessment. For details of local providers that conduct community assessments contact Direct line on 1800 888 236.
We are situated at number 9 Brunswick St, Fitzroy 3065.
Access to Depaul House is now through community assessment. For details of local providers that conduct community assessments contact Direct line on 1800 888 236.
Medical Services
- Specialist medical consultation services are available by appointment for individuals referred from their general practitioner.
Counselling Services
- Counselling services are offered to any person who has a problem with their own or someone else's drug or alcohol abuse.
- Individual treatment plans developed according to client's needs
- Referral to other services when required, eg withdrawal/residential program
- Counselling sessions are pre-booked
- We are not a crisis service, but we endeavour to see new clients as soon as possible after contact is made
The consultation/liaison service provides advice and care for all St. Vincent's inpatients with drug or alcohol problems who are referred to the service.
The service provides:
-
Medical management of alcohol or drug withdrawal
-
Management advice
-
Brief intervention/education on the effects of substance abuse
-
Advice on discharge planning.
Hospital patients can also be referred to community agencies and counselling for outpatient counselling/treatment for their drug or alcohol problem.
ECHO means Extension for Community Healthcare Outcomes. Project ECHO is a lifelong learning and guided practice model that
revolutionizes medical education and exponentially increases workforce capacity to provide  best-practice specialty care and reduce health disparities.
best-practice specialty care and reduce health disparities.
We are using ECHO to bring specialist knowledge and support in opioid management to health practitioners throughout Victoria.
We aim to cover all aspects of opioid management including prescription and illicit opioid misuse/abuse and addiction, opioids and addiction in chronic pain management, medication assisted treatments for opioid use disorder (MAT, MATOD, methadone,
buprenorphine), overdose, regulations and opioid prescribing, trauma-informed care, dual-diagnosis.
The heart of the ECHO model is its hub-and-spoke knowledge-sharing networks, led by the multidisciplinary team at the Department of Addiction Medicine at St Vincent’s Hospital Melbourne who use multi-point videoconferencing to conduct tele-support for community providers. In this way, primary care doctors, nurse practitioners, pharmacotherapy consultants and other clinicians learn to provide excellent specialty care to patients in their own communities.
For more information please contact Amanda Norman - Amanda.Norman@SVHA.org.au
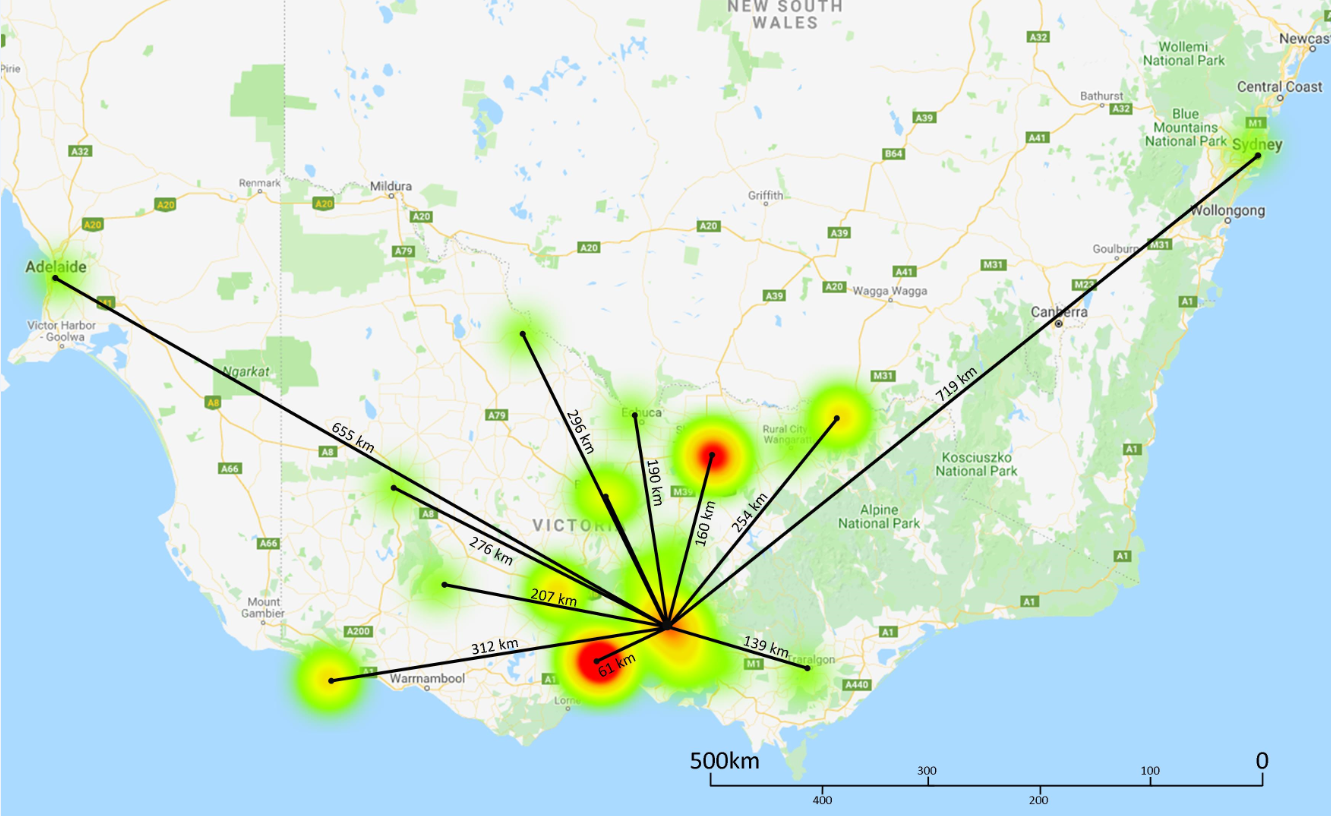
Heat map of Victorian Opioid Management ECHO's reach
Testimonials from ECHO participants:
“Hi Team,
Just giving feedback how much I am enjoying the ECHO sessions. Even though I have been a methadone prescriber for 23 years I have learnt a lot from the sessions. It is also helpful and reassuring to get the Hub's opinions on cases and I feel that my approach has become more systematic to my own patients since engaging with ECHO. This effect is magnified as I am a sort of backup resource about opioids and prescribing in Geelong and near surrounds. So a big THANK YOU and WELL DONE..”
GP, Geelong
“Such a complex case study but the suggested treatment plan was so applicable and the suggestions offered by (the psychiatry registrar) were brilliant and very culturally sensitive …. Overall a very informative and thought provoking session.”
Pharmacotherapy Co-ordinator, Gippsland
ECHO means Extension for Community Healthcare Outcomes
. Project ECHO is a lifelong learning and guided practice model that revolutionizes medical education and exponentially increases workforce capacity to provide best-practice
specialty care and reduce health disparities.
The heart of the ECHO model is its hub-and-spoke knowledge-sharing networks, led by the multidisciplinary team at the Department of Addiction Medicine at St Vincent’s Hospital Melbourne and the Pain Service at the Royal Melbourne Hospital who use multi-point videoconferencing to conduct tele-support for community providers. In this way, primary care doctors, nurse practitioners and other clinicians learn to provide excellent specialty care to patients in their own communities.
The curriculum will cover the following key learning objectives:
• Understand best practice management of patients with chronic pain.
• Understand the interdisciplinary dynamics of managing a patient on long term opioid medication.
• Able to apply a case-based learning approach to optimising assessment and treatment of a patient with chronic pain and opioid dependence.
• Able to safely and effectively prescribe Schedule 8 medications and other drugs of dependence.
For more information about the Pain and Opioid Mangement Echo (EPOM), you can download the flyer here.
Department of Addiction Medicine, St Vincent’s
Partner Provider Initiative
St Vincent’s Department of Addiction Medicine (DoAM) Partner Provider Initiative is part of the Collaborative network of Addiction Specialist services. The network is co-ordinated centrally by Turning Point and the state-wide addiction Specialist service collectively
operates under a broad umbrella name of “the Hamilton Centre”. The focus of the specialist service is to work with Area Mental Health & Wellbeing Services (AMH&WS), Local MH&WS and Residential Alcohol and Other Drug Services to build capacity in providing
better integrated care to people with co-occurring MH & Substance Use issues. Responses to inquiries will be provided within 72 hours (M-F) and planning of the consultation within 5 working days.
Referrals can be made through the Hamilton Centre website, email at info@hamiltoncentre.org.au or call 1800 517 383.
Should you require any further assistance, please do not hesitate to contact us on (03) 9231 6940 or email St Vincent’s at SVHM.PPI@svha.org.au.
St Vincent’s Hospital Melbourne and St Vincent's Private Hospital is committed to providing accessible parking across the campus for the convenience of patients, carers, visitors, staff, .and contractors.
St Vincent's, Building A - Main Hospital, Underground Car park
- Car Spaces - 240
- Disabled Car Space - 6
- Location - Acces to Basement, Building A - Main Hospital, via Fitzroy Street, Fitzroy, on your left
- Operational Hours - 6.30am - 10.45pm 24/7 card access
- Fees - Fees apply (see below)
- Who can park here? - Patients, Visitors, Staff
St Vincent's Fitzroy Street
- Car Spaces - 400
- Disabled Car Space - 2
- Location - Access via Fitzroy Street, Fitzroy on your right (please note, Fitzroy Street is a one way street access via Victoria Parade)
- Operational Hours - 6.30am - 10.45pm with an access card 24/7
- Fees - Fees apply (see below)
- Who can park here? - Patients, Visitors, Staff (St Vincent's Hospital Melbourne and St Vincent's Private Hospital)
St Vincent's Victoria Parade Car park
- Car Spaces - 515
- Disabled Car Spaces - 6
- Location - Access via 93 Victoria Parade, Fitzroy
- Operational Hours - 6.30am - 10.45pm 24/7 card access
- Fees - Fees apply (see below)
- Who can park here? - Provided for Staff and Childcare Drop off
Fitzroy Car Park Office is located in basement of Building A - Main Hospital.
Hours are:
- Mon to Fri 7:00am – 9:00pm
- Sat & Sun 9:00am – 5:00pm
Please Note: Any visitor entering the St Vincent’s Campus Car Parks will be deemed to have agreed to and accepted the St Vincent’s Car Park Terms and Conditions located at the entrance to the above Car Parks.
Parking Fees
(effective Monday 4 April 2016):
- 0-1 Hour - $10.00
- 1-2 Hours - $15.00
- 2-3 Hours - $18.00
- 3-4 Hours - $20.00
- 4-5 Hours - $23.00
- 5-6 Hours - $28.00
- 6+ Hours - $28.00
- Maximum Daily Rate - $28.00
- Weekend/Public Holiday rate - $12.00
- Concession - $11.00
Customers will need to pay for parking before returning to your vehicles and exiting the hospital car parks. This can be paid at the pay stations (cash or credit card) located next to the lifts on the lower level of each car park.
St Vincent’s Hospital Melbourne makes a number of provisions to meet the needs of our patients and carers. Car parking concession tickets are available for eligible patients and carers.
Pension Card Holders
Patients/ carers possessing a valid, in-date Federal Government Concession card with the patient or visitor name listed on the card are eligible for the concession parking. Patient or carer is to present their parking ticket along with pension card to the Car Park Office to obtain the concession parking rate.
Patients / Carers suffering Financial/ social hardship related to hospitalisation
Concession parking is available to:
- Patients experiencing prolonged periods of hospitalisation (20+) days and their carers to assist to mitigate the financial burden.
- The main carer if they are experiencing significant additional expenses related to hospitalisation/visits (e.g.: accommodation costs, travel costs).
How to get to the Fitzroy Campus
The Fitzroy campus, bordered by Nicholson Street, Victoria Parade, Fitzroy Street and Gertrude Street Fitzroy is well serviced by public transport.
Trams
Trams that stop at the corner of Nicholson Street and Victoria Parade are:
- 86 Bundoora RMIT – Waterfront City Docklands
- 96 East Brunswick – St Kilda Beach
Trams that stop at the St Vincent’s Plaza ‘super stop’ on Victoria Parade are:
- 11 West Preston – Victoria Harbour Docklands
- 24 North Balwyn – City (Latrobe St west end)
- 30 St Vincent’s Plaza – Etihad Stadium Docklands
- 42 Box Hill – Victoria Harbour Docklands
- 109 Box Hill – Port Melbourne
- 112 West Preston – St Kilda
*Any tram travelling up Bourke St will stop at St Vincent’s Plaza
Buses
Buses that stop near St Vincent’s on Victoria Parade include:
- 340 City – La Trobe University via freeway (all stops)
- 350 City – La Trobe University via freeway (limited stops)
- 402 Footscray – East Melbourne via North Melbourne
- 684 Eildon – Melbourne via Lilydale Station
Trains
The closest station to St Vincent’s is Parliament Station, a 10 minute walk from our Fitzroy campus across Victoria Parade. Any city loop train can be taken to Parliament station.
Trams including the 109, 112, 86 and 96 stop near Parliament Station and will drop you at our Fitzroy campus.
Visit www.ptv.vic.gov.au for more information.
Taxis
Taxi phones (free call) are located in the foyers of the Emergency Department, St Vincent’s Clinics and Building F - Bolte Wing.
Contact
62 Gertrude Street, Fitzroy, VIC 3065
Tel: (03) 9231 6940
Fax: (03) 9231 2642
For information about how to make a referral click here.