It is your responsibility as students to be aware of your scope of practice at all times. If you are delegated tasks outside of your scope of practice you are to decline and inform your clinical teacher. Any practices outside of your scope of practice will automatically award you a fail for your clinical placement, your education provider will be informed and relevant incident reports completed.
Debriefing and education sessions will be arranged according to your placement type, year level and groups experiences. As a rule debriefing sessions are pre-arranged weekly and extra sessions are added throughout the week. We do not enocourage our teachers to run group sessions each day as its important that you complete your hours in a clinical context, as well as gain an understanding of the role and responsibilities of nurses aross an entire shift.
Ward computers are available to all clinical staff to assist in the care of our patients. Additional computers are available on our Fitzroy campus at our Library for students to use
When administering medications you must ensure:
- The right patient
- The right medication
- The right dose
- The right route
- The right time
- The right expiry date
- The patient allergy history
- The right reason (to give or withhold)
Students MUST be supervised at all times while preparing and administering medications.
Students MUST administer medications under the supervision of a Grade 2 Year 2 or above, nurse.
Students are NOT PERMITTED to administer medications with a Graduate Nurse or Agency Nurse.
Within scope of practice, undergraduate nursing students are permitted to administer medications under the direct supervision of a:
- Clinical Teacher directly responsible for that student who is a SVHM Registered Nurse seconded to the role
- Clinical Teacher directly responsible for that student who is a Registered Nurse employed by the education institution where the student is enrolled
- Medical Practitioner
- Pharmacist
- SVHM Registered Nurse Grade 2 Year 2 or above
Exceptions to this are:
- All injectable medications (intravenous, subcutaneous, intramuscular) except subcutaneous heparin
- Schedule 8 medications (S8 Drugs of Addiction)
- Schedule 11 medications (S11 Drugs of Dependence)
- Oral anticoagulants
- PRN medication
- Nurse initiated medication
For these administrations the student must be under the direct supervision of a SVHM Registered Nurse (Grade 2 Year 2 or above) responsible for that patient or a Clinical Educator who is a SVHM Registered Nurse seconded to the role. All medication administration must be double checked according to the requirements outlined in the Hospital Medication Policy.
Enrolled Nurses (Enrolled Nurse Students) are not permitted to administer nurse initiated medications.
If a student is administering medications with their clinical educator and the patient refuses medication, it is the responsibility of both the student and the clinical educator to inform the nurse responsible for the patient, as well as document this on the medication chart and in nursing notes
If a student is administering medications with their clinical educator and the patient is fasting, the student and clinical educator must speak directly to the nurse responsible for the patient in regards to which medications should be administered or withheld
If unsure of the correct administration of any medication please refer to:
- Ward Pharmacist
- MIMS and MIMS Online
- St. Vincent’s Hospital Drug Administration Protocols
Abbreviation: MANE
- Definition: Morning
- Usually Given: 8.00am
- Note:
Abbreviation: MID
- Definition: Midday
- Usually Given: 12.00pm
- Note:
Abbreviation: NOCTE
- Definition: Night time
- Usually Given: 8.00pm
- Note: 10.00pm sedation at night
Abbreviation: D or Daily
- Definition: Once per day
- Usually Given: 8.00am
- Note: Exceptions may apply
Abbreviation: BD
- Definition: Twice daily
- Usually Given: 8.00am/8.00pm
- Note: Exceptions may apply
Abbreviation: TDS
- Definition: 3 x daily
- Usually Given: 8.00am/2.00pm/8.00pm
- Note: Need to specifically want 8 hourly (see below)
Abbreviation: QID
- Definition: 4 x daily
- Usually Given: 8.00am/12.00pm/6.00pm/10.00pm
- Note: Need to specifically want 6 hourly (see below)
Abbreviation: Every 8 hours
- Definition: Eight hourly
- Usually Given:
- Note: Use only when dosing a regular intervals is required
Abbreviation: Every 6 hours
- Definition: Six hourly
- Usually Given:
- Note: Use only when dosing a regular intervals is required
It is a medical responsibility to document medication administration time
You must:
- Date and Time EVERY entry
- Print your surname, designation and signature for EVERY entry, countersigned by your buddy nurse
- Have a patient ID on every page (UR Sticker or written UR number and surname)
- Be brief, factual, objective
- Use neat and legible writing
- Write notes sequentially
- Make note of errors by drawing a single line across the appropriate area, with “Entry made in error” written, and signature
- Not destroy or delete any document
- Draw a single horizontal line through any unused writing space
- Use black or blue pen only
- Not use highlighters/fluorescent markers or liquid paper
How often should you document?
- Daily (on AM shift)
- At any time of a significant clinical change in condition ie. transfer or post operatively
The sub-acute clinical areas utilise ‘Record of Patient Care’ care plans which are completed daily (usually on AM shift) and signed off by the nurses on the PM and night shifts. The tool is used to record care required and provided, however any variances from the tool or additional information that does not fit within the tool must be documented in the patient’s progress notes.
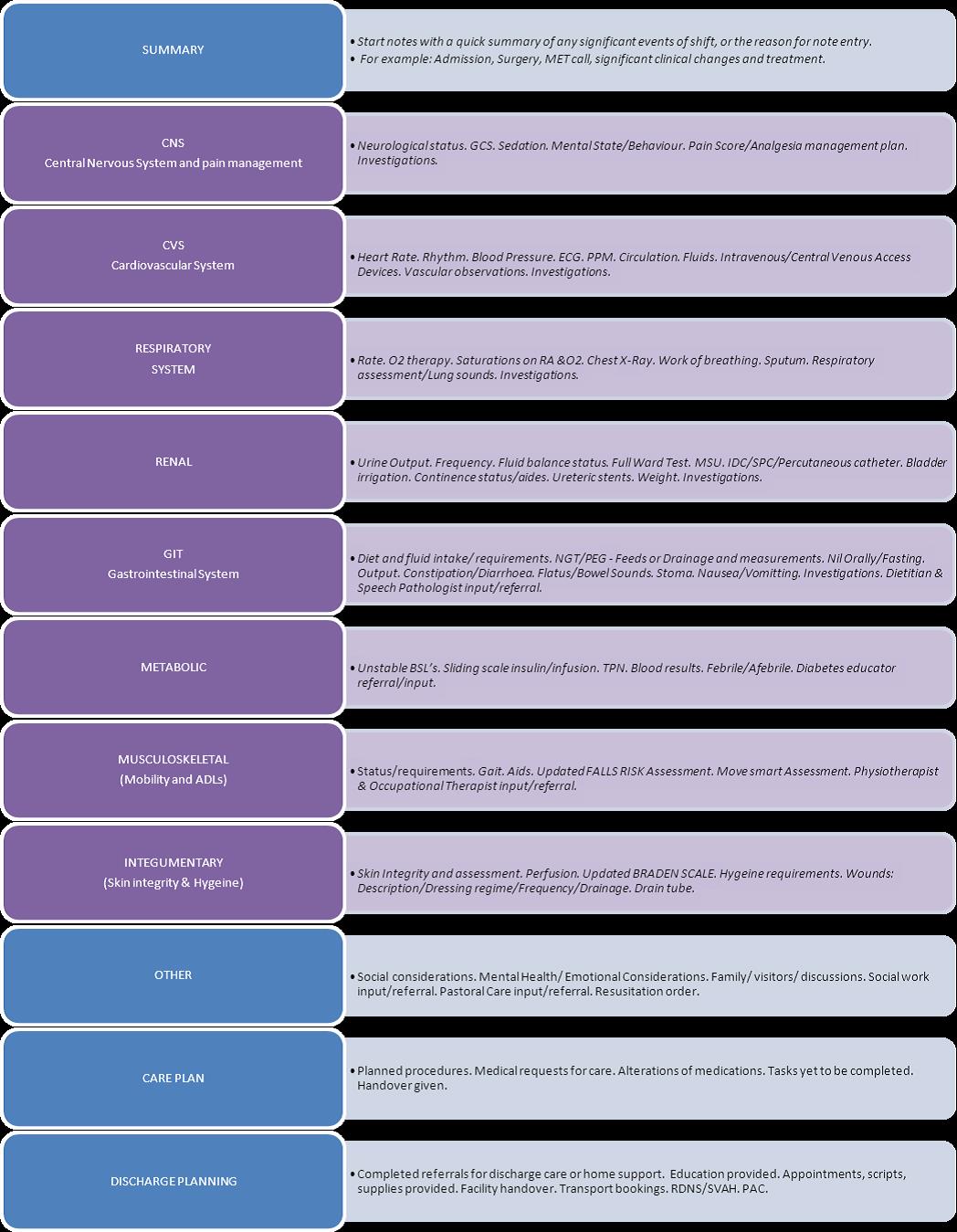
SVHM Nurses follow a systems approach to documentation that we ask you follow when writing your notes.
Systems Approach to Documentation
You can use the following table as a guide:
Your hand over should take no longer than 4-5 minutes. Be brief and to the point.
What to include
- Bed number
- Patient’s name
- Abnormal Vital signs
- Abnormal Blood sugar levels
- Abnormal Blood results
- Oxygen saturations
- Mobility and ADL status e.g. RIB,Transfer with 2, requires feeding
- Oxygen therapy
- Venous access e.g. IV bung, CVC, PICC
- Incontinence/constipation
- NG/PEG feeds
- Drain tubes
- Wounds
- Pain control
- Procedure/tests and outcomes
- Administration of blood products
- NFR orders
- Catheters e.g. IDC, ICC
- It is enough to state that the patient is receiving IV antibiotics/fluids
- Health care problems
- Discharge plan
What not to include
- Diagnosis
- Past history
- Age
- Normal Vital signs
- Normal Blood sugar level
- Normal Blood results
- Normal Oxygen saturations
- Usual medications/treatments
- Routine care
- Frequency of vital signs
- Weighs
- Urinalysis
- Type, time & rates of IV antibiotics/IV fluids
- Referrals/consults
NB. It is only essential to state patients’ diagnosis and past history if it does not appear on the handover sheet
As a student you will have tasks delegated and supervised by nursing staff. It is essential that you understand your responsibilities in accepting these tasks. The FAQ sheet via the link below details your responsibility in the delegation process and a video example has also been attached specific to students.
Delegating to Undergraduate Student Video
Codes are a frequent part of life at SVHM and it’s important to understand that the Emergency Management System we have in place is equipped to prevent, prepare, respond and recover from any emergency. In the event that a code is called within your area or for your patient you need to follow the instructions of your buddy nurse and allow our team to put our emergency procedures into place.
Click here for link to St Vincent's Emergency Codes table.
Prevention & Management
- All patients must be assessed for risk by the admitting nurse using the Nursing Risk Admission Form. All patients who screen positive (i.e. Patient > 65 years, previous history of falls or nurses deems patient to be at risk of fall) must have a falls risk assessment completed using the Northern Health – Stratify Falls Assessment form
- All patients who are deemed High risk must have a management plan completed and interventions applied according to risk factors
- This form should be placed in the bedside chart and be updated if a patient has a fall, if there is a change in patient condition or environment (i.e. transfer)
Patients who are identified as a falls risk should have a falls alert placed:
- Above their bed
- On the handover sheet
- On their walking aid
-
On PAS
- High risk patients should be transferred to a hi-lo bed
If your patient has a fall:
- Your buddy nurse, the nurse in charge and medical staff must be notified immediately
- Perform a set of neurological observations and vital signs, and help to return patient to bed with assistance from other nurses, using Move Smart equipment, if safe to do so
- Continue regular observations as ordered
- A VHIMS incident report must be completed following all falls, speak to your buddy nurse about this
- Document a fall in the patient history and reassess the patient’s falls risk on the falls risk screening tool
- Notify NOK
- The Move Smart Program aims to reduce the risk of musculoskeletal injuries that are attributed to the manual handling of people through the provision of NO LIFT techniques and equipment, and education for staff
- The Move Smart Co-coordinators are available Monday to Friday and can be contacted for assistance with any Move Smart inquiries
- A Move Smart Assessment form should be completed on patient admission and as patient condition changes, identifying supervision and mobility equipment required for each patient
- This form must go with patients when they leave the ward, ie. Medical Imaging, theatre
DO NOT MOVE ANYTHING OR ANYONE WITHOUT SPEAKING TO SOMEONE FIRST
Needle stick injuries or a splash of blood or body fluid to non-intact skin and mucous membranes are termed Occupational Exposures.
It is essential that all these incidents be reported IMMEDIATELY when they occur, as treatment may need to be initiated within 2 hours of the incident.
For all Occupational Exposures you need to page 777 if at St Vincent’s Fitzroy Campus, 2820 at the St. George’s Campus or phone 5607 if at Caritas Christi, 24 hours a day 7 days a week. The Occupational Exposure Coordinator will come to you and manage the incident.
Please remember to complete the details of the incident in an online incident form (VHIMS Riskman™).
The Clinical Educator is responsible for informing the University of Occupational Exposures involving students and may need to complete a separate Incident form if required by the educational institute.
Patients, Visitors, Staff & Students
If you witness or are informed of an adverse event involving a patient or visitor it is your responsibility to alert your allocated buddy/preceptor or Nurse in Charge.
An allocated staff member will fill out an online incident form using the VHIMS Riskman system.
For all incidents involving a student, a University incident report needs to be completed in addition to a hospital incident report.